GASTRIC BALLOON
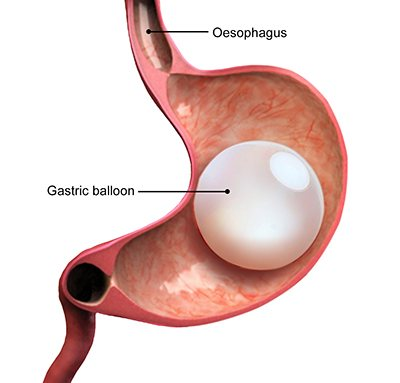
Intragastric balloon placement is a weight-loss procedure that involves placing a saline-filled silicone balloon in your stomach. This helps you lose weight by limiting how much you can eat and making you feel full faster. Placing an intragastric balloon is a temporary procedure that does not require surgery.
The intragastric balloon procedure may be an option if you have concerns about your weight, and diet and exercise haven’t worked for you.
Like other weight-loss procedures, an intragastric balloon requires commitment to a healthier lifestyle. You need to make permanent healthy changes to your diet and get regular exercise to help ensure the long-term success of the procedure.
Why is this treatment needed?
When you have obesity, your body changes in ways that make it increasingly hard to lose weight by diet and exercise alone. One of those changes is that the volume of your stomach expands over time. As your stomach stretches, it holds more food and takes longer for you to feel full, which leads to eating more. This is why all medical weight loss procedures restrict the capacity of your stomach by some means. The intragastric balloon offers an important alternative to the other available procedures. First, it’s the only procedure that’s designed to be impermanent. Second, it doesn’t require surgery to install it. It doesn’t require general anesthesia, either. This makes it a viable option for those who either don’t meet the qualifications for bariatric surgery or are looking for a lesser commitment.
 Who is intragastric balloon therapy for?
Who is intragastric balloon therapy for?
In the U.S., the intragastric balloon is currently offered to people with a BMI of at least 30 who pass the health screening for the procedure. People with class III obesity who qualify for bariatric surgery may choose the balloon instead for its relatively low risks. People whose obesity makes surgery unsafe for them may use the balloon as a bridge procedure to lose enough weight to qualify for surgery.
What health conditions does the intragastric balloon treat?
Obesity causes metabolic changes that lead to a wide range of health conditions, from Type 2 diabetes and cardiovascular disease to kidney and liver diseases. If you have a BMI of 30 or more, you’re at a high risk of developing these diseases. But on the flip side, weight loss of just 5% to 10% reduces this risk and can even cause remission of these conditions. You can achieve this with the intragastric balloon system.
How much weight can you lose with a gastric balloon?
Average weight loss with the gastric balloon is about 10% of your total weight or about 30% of your excess weight. That’s enough to make a life-changing impact on your health in a short period. As with any weight loss system, you can lose more or less depending on how well you stick to the program. You can also regain the weight you lost if you don’t stick to the program after the balloon is removed.
What happens before intragastric balloon placement?
You’ll consult with your healthcare provider to determine if you’re a good fit for the intragastric balloon system. If you are, your healthcare provider will assemble a team of caregivers to support you through the program. You’ll consult with a nutritionist, gastroenterologist, psychologist/psychiatrist and possibly others to design a personalized weight loss program.
Who shouldn’t have the gastric balloon?
Your healthcare provider may not advise it if you have:
- Peptic ulcer disease.
- Hiatal hernia.
- A blood clotting disorder.
- Liver disease.
- Substance use disorder.
- A history of previous gastrointestinal surgery.
How will I be prepared for the procedure?
A healthcare provider will explain the risks, benefits and alternatives to the procedure and obtain your informed consent to proceed. They’ll often start you on acid-blocking medication to prevent acid reflux during and after the procedure. A few days before the procedure, they’ll put you on a clear liquid diet to help empty your stomach. The night before, they’ll ask you not to eat and drink anything after midnight.
How is the intragastric balloon inserted?
Healthcare providers insert most intragastric balloons using an endoscope. An endoscope is a long, flexible tube with a camera attached. It goes in through your mouth and passes down through your esophagus to reach your stomach. Most people have this procedure while awake, but with a mild sedative. (The Obalon® is a newer balloon that you can swallow, but it still has to be removed by endoscope.)
 What happens during the intragastric balloon procedure?
What happens during the intragastric balloon procedure?
You’ll have medication to help relax you and numb your throat for the endoscope. Your gastroenterologist or endoscopic surgeon will begin by examining your esophagus and stomach with the endoscope, which projects images onto a screen. Once they’re satisfied that you don’t have any conditions that could make the balloon unsafe, they’ll guide the balloon into place.
The Orbera balloon is filled with a sterile, saline solution, as most models are. The Obalon — as well as some others available outside of the U.S. — is filled with gas. Providers don’t use gas-filled balloons as often because they aren’t as effective overall for weight loss, but they can be more comfortable. Providers recommend them for certain people and circumstances, based on their characteristics.
Your endoscopist will fill the balloon with a syringe attached to the catheter, then detach the syringe and withdraw the catheter. The valve on the balloon seals to prevent leaks. The filled Orbera balloon takes up about a third of your stomach. The weight of the fluid makes it sink to the bottom, which is part of how it works. It slows down the emptying of your stomach through the valve at the bottom (pylorus).
The procedure itself takes 20 to 30 minutes. Afterward, you’ll spend a few hours recovering in the hospital. You’ll have IV fluids and medication to prevent pain and nausea. Your healthcare team will make sure you’re tolerating the balloon before they discharge you. They’ll also leave you with dietary instructions to follow in the weeks ahead. You’ll stay on a clear liquid diet for the rest of the day.
What happens after the procedure?
Your stomach will need time to adapt to the balloon before you resume your regular diet. You’ll start with a liquid diet and gradually advance to pureed foods, followed by a soft diet, and finally, the long-term diet designed by your nutritionist. You’ll stay in close contact with your healthcare team during this time. They’ll support you through the physical and psychological side effects while you’re adjusting.
How long does an intragastric balloon last?
The Orbera balloon stays in place for six months. During this time, you’ll continue to work with your team to make the diet and lifestyle changes that will sustain your weight loss over the long term. You’ll eat less, lose weight and retrain yourself to notice when you’re getting full. You’ll continue acid-blocking and anti-nausea medications as needed. The greatest weight loss happens in the first three months.
What happens when the balloon comes out?
You’ll have a second endoscopic procedure to remove the balloon. You’ll be given a sedative and a topical anesthetic or lubricant in your throat to ease the removal. Your endoscopist will puncture the balloon, suction out its filling and then withdraw the deflated balloon. After the balloon comes out, your team will continue to work with you for six more months to reinforce your long-term lifestyle changes.
What are the side effects of the intragastric balloon?
Side effects of mild gastrointestinal symptoms are common, and healthcare providers often prescribe medication to prevent or manage them. Symptoms usually only last a week or so, but sometimes longer. They include:
- Temporary abdominal pain.
- Temporary sore throat.
- Nausea.
- Indigestion.
- Acid reflux.
- Constipation.
How painful is it?
It’s usually more of a dull discomfort than acute pain, and it usually doesn’t last. Some people experience more noticeable pain during the first week after the procedure, but it’s manageable with medication.
What are the risks of a gastric balloon?
Serious complications are rare, but they can occur. The risks include:
- Persistent gastrointestinal symptoms. Less than 3% of people have persistent symptoms that go on beyond the first week and that aren’t relieved by medication. These people will need another endoscopy to investigate the problem and either adjust the balloon or remove it.
- Hyperinflation. A little over 2% of people experience spontaneous hyperinflation. During hyperinflation, the balloon malfunctions and overfills itself sometime after the first inflation. This can cause persistent gastrointestinal symptoms, leading to early removal of the balloon.
- Deflation. If the balloon ruptures or deflates, it can migrate out of your stomach and into your intestines. The risk of this is about 1.5%. Different intragastric balloons have different tracking devices to alert you and your healthcare team if this happens. Most balloons that migrate into your intestines will pass safely through, but there’s a risk that a balloon could get stuck there and cause an intestinal obstruction. This would require an emergency procedure to remove it.
- Acute pancreatitis. The FDA has received about 20 reports of acute pancreatitis resulting from the Orbera balloon. They speculate that pressure from the balloon inside your stomach may impinge on your pancreas behind it, causing inflammation. Acute pancreatitis is often painful, and a severe case can be serious. If the balloon is the cause, you’ll need to have it removed.
- Ulceration. Intragastric balloons are made of soft silicone, smooth and round to contour to the shape of your stomach. This is to prevent the balloon from irritating your stomach lining. But stomach ulcers have occurred, probably due to pressure where the balloon rests at the bottom of your stomach. Some people also get ulcers in their esophagus due to injury during balloon placement or removal. The most serious risk of an ulcer is that if it doesn’t heal, it can eventually wear all the way through your gastrointestinal lining, leaving a hole (perforation). This can lead to a life-threatening infection. The risk of gastrointestinal perforation is 0.1%.