SLEEP APNEA SURGERY
What Is Surgery for Sleep Apnea?
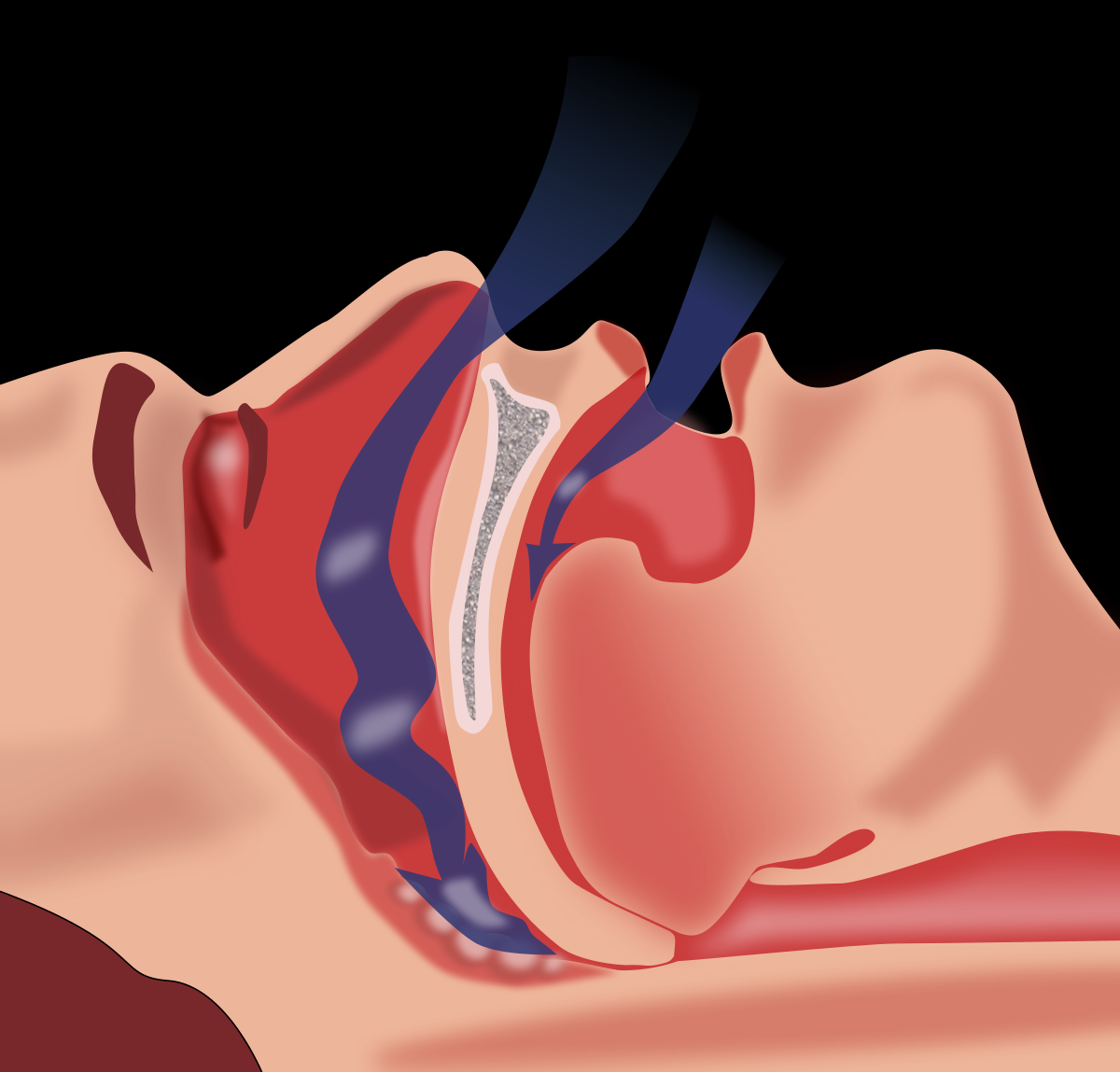
There are many surgeries given to people with obstructive sleep apnea (OSA)and one for people with central sleep apnea (CSA).With OSA, a person stops breathing during sleep because their airway becomes partially or completely blocked. Surgeries for OSA primarily involve reducing physical blockages, for example by removing tissue or adjusting placement of the jaw or tongue. The ideal surgery for a given individual with OSA depends on their anatomy and what is causing their airway blockage. Sometimes weight loss surgeries are also recommended, since OSA and obesity are linked.
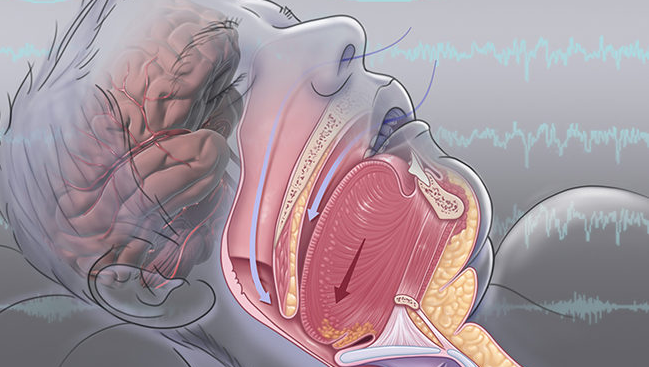
With CSA, a person stops breathing during sleep due to a problem with signals sent from the brain stem. Because CSA-related lapses in breathing are not caused by physical blockages, surgeries for OSA would not work as a CSA treatment. However, there is one surgical procedure available for people with CSA that involves electrically stimulating a nerve that leads past the lungs to the diaphragm.
Before recommending a type of sleep apnea surgery, a medical professional generally conducts a pre-surgical evaluation. This evaluation often involves a nasopharyngoscopy, or a short procedure in which a flexible scope is inserted into the nose and throat, allowing the doctor to look for areas that might cause blockages while sleeping.Sometimes pre-surgical evaluations involve a sleep endoscopy, in which a scope is inserted into the nose and throat while a person sleeps. In certain cases, a doctor may also order scans, such as a computed tomographic (CT) scan, a magnetic resonance imaging (MRI) scan, or an x-ray to look for blockages.
The medical team will choose the best surgery depending on what they find, and may perform more than one surgery on different areas.
How Is Sleep Apnea Diagnosed?
In order to confirm that someone has sleep apnea, a test called “Polysomnogram” is required. This test consists of multiple tests that monitors, records and transmits the body’s activity during sleep. Some surface electrodes will be placed on the person’s forehead and scalp to record electric signals, and two belts, one around the waist and the other around the chest to monitor and record the breathing pattern. An oximeter is placed on a finger for measuring the existing amount of oxygen in the blood while sleeping. The health professional will then study and analyze the records and decide whether the person has sleep apnea or not. This test can be performed, in a lab, in a hospital or even at the comfort of someone’s home.
How Is Sleep Apnea Treated:
There are both natural treatments and devices- or surgery-based treatments for sleep apnea. Natural treatments include lifestyle changes in general, such as weight loss, quitting smoking, quitting drinking, etc.
Here we will only name the treatments and discuss more the various sleep apnea surgeries.
Other options for sleep apnea treatment include:
- CPAP (continuous positive airway pressure) which refers to keeping the airways open and by a gentle and constant stream of positive pressure air is breathed through a mask.
- MRD (Mandibular repositioning device) which increases the space behind the tongue by holding the jaw in a forward position. Side effects of this treatment may include, tooth and jaw pain.
- Surgery: Numerous surgeries are performed to widen the airways, remove the obstructing tissue, remove enlarged tonsils.
Sometimes the person may need to undergo both surgical and non-surgical treatments.
Surgical Treatments for Sleep Apnea (SOMNOPLASTY)
- Uvulopalatopharyngoplasty (UPPP):
This type of sleep apnea surgery is the operation of the anterior surface of the soft palate and targets the back of the roof of the mouth. During this procedure, the excess tissue in the throat will be repositioned and removed in order to make the airway wider. The soft palate and uvula can be trimmed and pharyngeal arches and the tonsils may need to be removed and some of the muscles of the throat repositioned by the surgeon. In this surgery, the uvula is folded towards the soft palate.
The downside of UPPP is that, although it is the most commonly used type of procedure for sleep apnea treatment, it will not cure the moderate to severe cases of sleep apnea, and the person may need to undergo surgeries of upper respiratory system that targets other sites in the upper airways, or they might also need to continue using non surgical treatments.
UPPP surgery unpleasant side effects
- Swallowing difficulties
- Speech problems
- Taste disturbances
- Smell disturbances
- Velopharyngeal insufficiency
- Nasal regurgitation
- Oral pain, swelling, infection, bleeding
- Mouth dryness
- Sleepiness and periods of not breathing which are not related to sleep apnea itself, and are directly related to the medicines that are being taken for pain relief.
- Narrowing of the air ways in the nose and throat
- Radiofrequency volumetric tissue reduction (RFVTR):
This radiofrequency ablation is used for mild to moderate cases of sleep apnea. In this procedure, the tissue around the throat will shrink and tighten by controlled cauterization method. This can also be performed on tongue, tonsils and soft palate.
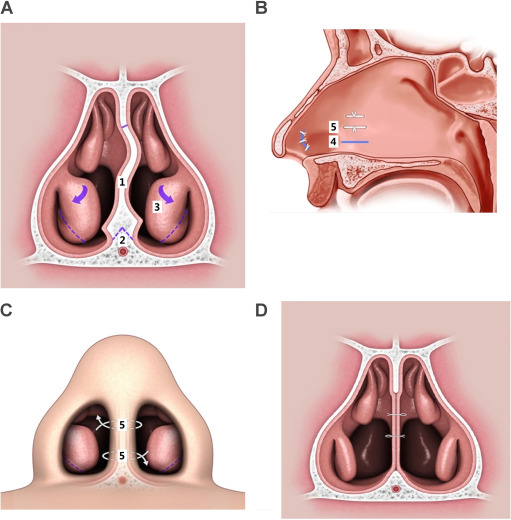
- Septoplasty and turbinate reduction
– Septoplasty
Septoplasty is widely used to help with the obstruction of the nose. Septoplasty is sometimes an essential part of other surgeries such as sinus surgery or nasal tumor removal. The septum is the divider between the two sides of the nose and is made of bone and cartilage. This bone and cartilage is covered with a layer of mucosa, which acts like a skin for the inside of the nose and protects the bone and cartilage. When the septum is deviated, it can block the nose. With these two procedures, the nasal passage is opened and airflow through the nose is improved, by straightening the deviated nasal septum, which means straightening the bone and cartilage. During this sleep apnea surgery, the mucosa has to be lifted in order to allow access to the bone and cartilage. The cartilage and bone can be reshaped and sometimes some parts of it has to be removed, and then the lining (mucosa), is laid back down. This part of the nose, the septal cartilage, has memory so it may assume it’s the previous shape, and bend back to its original shape after the surgery. This sleep apnea surgery is done in the operating room and under anesthesia. This operation is usually done under general anesthesia but if there is an option for local anesthesia the doctor will discuss that with the patient and help him/her decide which option to choose.
Septoplasty post-op care
There will be pain, nasal stuffiness and a mild nasal drainage after the surgery but the pain tends to be mild and can be controlled by taking oral pain medications. The reason for a feeling of stuffiness is swelling inside the nose after the surgery, which will gradually improve after the surgery. The drainage is mucous and blood which is normal during the healing process. As post-surgery care, it may sometimes be needed to use saline sprays and irrigations, but these and other post-operative cares must be instructed by the doctor.
- Turbinate reduction
Turbinates are the curved structures inside the sides of the nose, which are made of bone and soft tissue. Soft tissue or bone might be enlarged for a number of reasons, such as allergies. The most bothering situation is when the soft tissue is enlarged and swollen and it’s called hypertrophic turbinates. Medical options are also available to help reduce the size of turbinates. But the other option is the turbinate reduction surgery.
In many cases, turbinate reduction and septoplasty are done alongside each other. In the turbinate reduction surgery, it’s important not to remove all of the turbinate, because it will indeed affect the function of the turbinates and complete removal of it results in a crusty and very dry nose. Turbinate can grow back after the surgery, so the operation may need to be repeated if necessary. Some turbinate reduction surgeries do shrink the size of the turbinate without removing the soft tissue or turbinate bone. Operations such as cauterization, coblation, and radiofrequency reduction. In these procedures, a part of the turbinate is heated up with a special device. Gradually the scar tissue takes the shape of the heated part of the turbinate and causes the turbinate to shrink in size. With other procedures, a part of turbinate is removed, but it’s important to leave a significant amount of turbinate intact, to help humidify and warm the air that passes through the nose.
Post-op turbinate reduction surgery
Just like septoplasty, the patient can expect nasal stuffiness, pain, fatigue and nasal drainage. The pain can be controlled with normal pain medications, the stuffiness comes from swelling of the inside of the nose, and the drainage is related to blood and mucus coming out of the nose, which is also normal in the healing process.
Septoplasty and Turbinate reduction risks
- Tooth and nose numbness
- Infection
- Toxic shock syndrome
- Bleeding
- Persistent symptoms
- Septal perforation
- Spinal fluid leakage
- Genioglossus Advancement (GA)
The tongue is composed of muscles. These muscles can relax while sleeping and fall back and causes blockage in the throat and tongue area. Genioglossus is the largest muscle of the tongue, located in the center and is attached to the lower part of the jaw and below the teeth.
In this procedure, a small hole or bone cut is made in the front part of the lower jaw. This bone cut along with the genial tubercle is moved forward and is attached to the lower jaw, either by a single screw, plate or a number of screws. This sleep apnea surgery is done alongside other sleep apnea surgeries and treatments and it’s rarely done on its own for treating this sleeping disorder.
Genioglossus advancement recovery and post-operative care
Most patients can leave the hospital in a few days. Some recovery considerations must be done:
- Sleeping at a 45 degrees angle for a few days
- Sticking to a liquid or soft food diet in the first few weeks after surgery
- Drinking enough water and fluids to avoid dehydration, as painful as it might be
- Taking pain medication
- Avoiding heavy exercise and activities but maintaining a light routine of activity such as walking, to prevent any complications
- Hyoid Suspension
Hyoid suspension is also known as hyoid myotomy or hyoid advancement is another type of sleep apnea surgery. There’s a U-shaped bone in the neck, the tongue and other parts of the throat is attached to it. In this procedure, the hyoid suspension is pulled forward and secured in a proper place.
Hyoid suspension side effects
Side effects of this surgery include:
- Lip and chin anesthesia
- Seromas
- Edema
- Transient dysphagia
- Aspiration
- Surgical site infection
- Midline glossectomy (lingualplasty)
In some cases of sleep apnea, it’s advised to remove a part of the back of the tongue with a surgery called midline glossectomy or submucosal lingualplasty. This procedure prevents blockage of the airway by making the tongue smaller and is done under general anesthesia.
Except for a small incision on the neck for placing a plastic drain, there are no other external incisions and this surgery is done through an open mouth.
These two surgeries are not common.
- Midline glossectomy and lingualplasty side effects
- Bleeding
- Infection
- Tongue numbness and tingling
- Trouble swallowing
- Tongue weakness
- Tooth injury
- Need for additional surgeries
- Nausea and constipation
Midline glossectomy and linguaplasty recovery and post-op care:
- The patient is usually discharged after one or two days
- Ice in the mouth may help with pain and swelling reduction for the first 2- 3 days after the operation
- Drinking enough fluids is recommended
- Antibiotics can be used to prevent infection of the surgery site during the post-op period
- Patients should avoid strenuous activity
- Sleeping at 45-degree angle is helpful
- Postoperative appointments are vital
- Maxillomandibular osteotomy (MMO) and advancement (MMA)
This type of sleep apnea surgery is used for severe cases of sleep apnea. Maxillomandibular advancement or orthognathic surgery which is sometimes called bimaxillary advancement, or maxillomandibular osteotomy, is a sleep apnea surgery which moves the maxilla (upper jaw) and the mandible (lower jaw) forward. This surgery is usually done simultaneously with genioglossus procedure.
This procedure involves cutting a part of the jaw which will heal over time and in the course of months. The patient’s jaw will be wired shut for a few days after surgery.
This sleep apnea surgery is the most effective surgery for sleep apnea, but it’s usually not the first option and is chosen after previous failed treatments. Recovery time for this procedure is usually longer, comparing to other sleep apnea surgeries. This surgery is more difficult for the surgeon to perform, and the recovery process is also difficult for the patient.
- Palatal implants (pillar implants)
This sleep apnea surgery is used to cure snoring and in people with mild sleep apnea. This procedure can be done under local anesthesia and conscious sedation and in the doctor’s office. Tiny pillar implants, about 18 millimeters in length and 1.5mm in diameter, are inserted on the soft palate, preventing airway blockage by stiffening the tissue. This procedure is simple and effective.
- Weight loss surgery as a sleep apnea treatment
Bariatric surgery is recommended for obese people who also have other health concerns and simultaneously helps with sleep apnea (OSA) problem.
- Laser-assisted uvuloplasty (LAUP)
The surgeon tightens the soft palate by making cuts to the rear of the mouth and on the soft palate using a laser. With this procedure, a part of the uvula will be removed and is trimmed over several visits to the doctor. The advantages of this procedure are:
- It’s done in the doctor’s office
- It’s less painful than UPPP
- It has less side effects than the UPPP
- The disadvantage of this procedure is that it’s less effective.
- Tracheostomy (or tracheotomy)
In this sleep apnea surgery an alternative airway is provided by surgically creating a hole in the windpipe (trachea). Then a trachea tube is place inside the hole and is secured by a strap around the patient’s neck. This procedure is really effective but because of the invasive nature of this operation, it’s rarely chosen as the first option of treatment unless other treatments have been failed and this is the only remaining option. During the day, the tube can be inserted to help the patient with breathing and at night it can be opened and let the patient breath on their own and without any blockage in the throat.